

Lady presented to us by our musculoskeletal oncology specialist with suggestion of possible joint replacement of the right hip after resection for what was diagnosed as chondrosarcoma of the right acetabulum. All investigations confirmed the feasibility of wide resection with free margin which would allow a good field for hip implantation compatible with good survival. The question was whether such a resection would leave enough good bone stock for reconstruction with out standard reconstructive technique or whether we need a special implant.
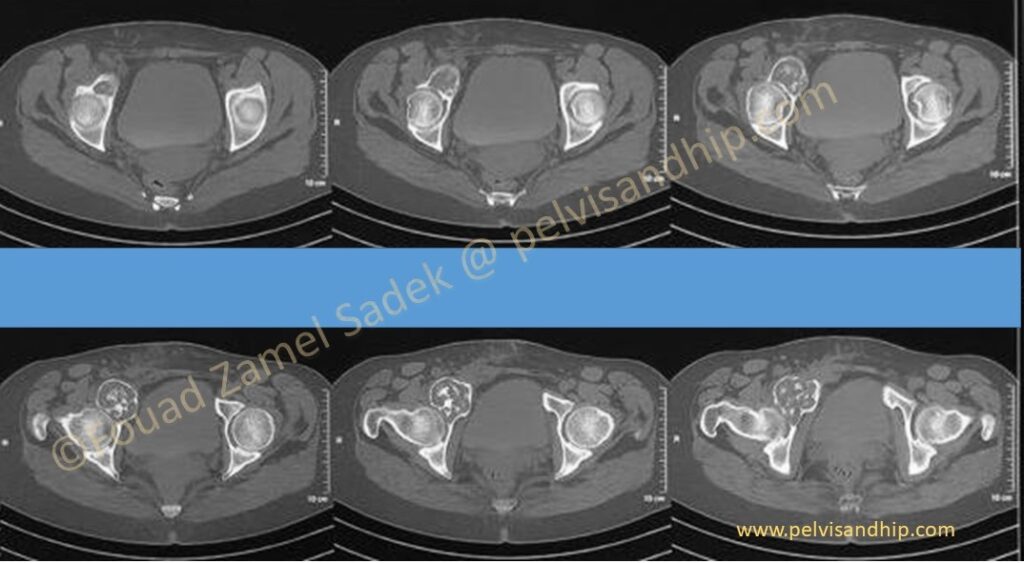
The axial CT scan cuts shows the tumour as it emerges from the anterior wall of the acetabulum with encroachment on the anterior joint space and extending to the superior pubic ramus.
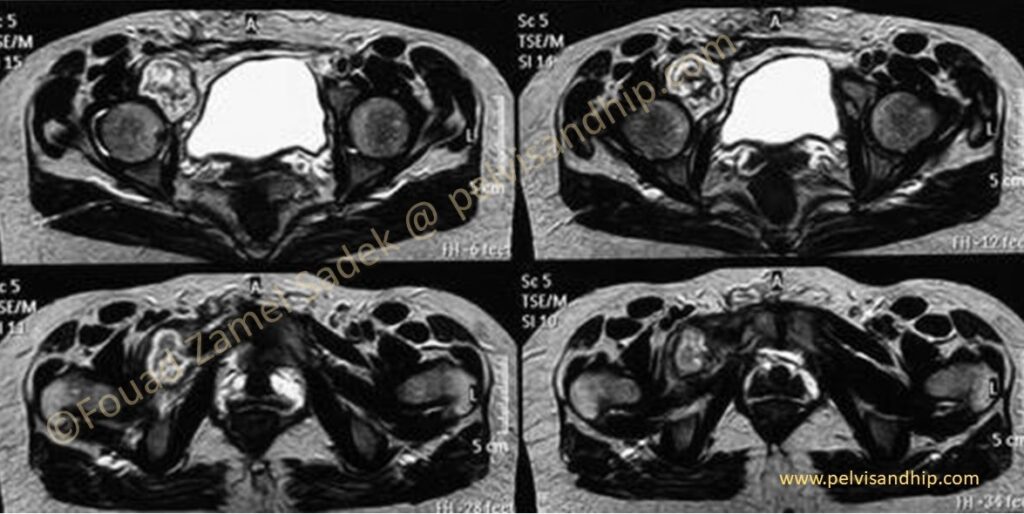
The MRI shows the localization of the tumour with resectable margins.
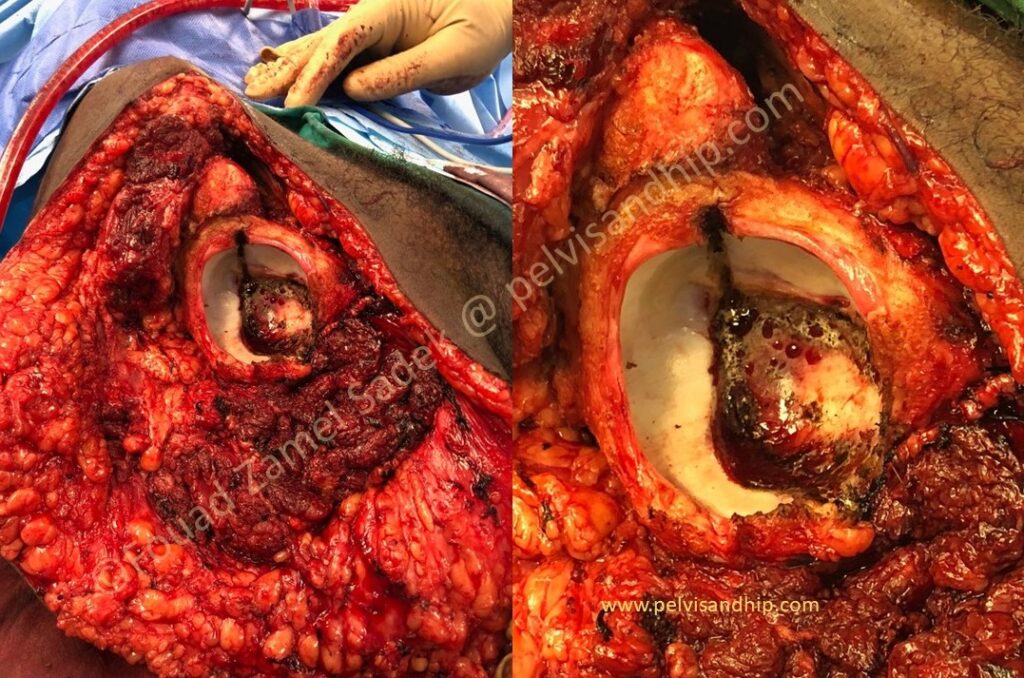
This intraoperative picture was sent to us by our colleagues taken during a disarticulation of another patient whereby the diathermy mark was made to give us an idea about the type of resection that would be done for that patient. Preliminarily, we will have the posterior half of the acetabulum; as far as this projected resection, for the cup implantation in the event of a total hip replacement.

Resected specimen after the surgery with the outer aspect on the right side showing the removed part with the inner side of the specimen whereby one can see the skin island including previous biopsy.
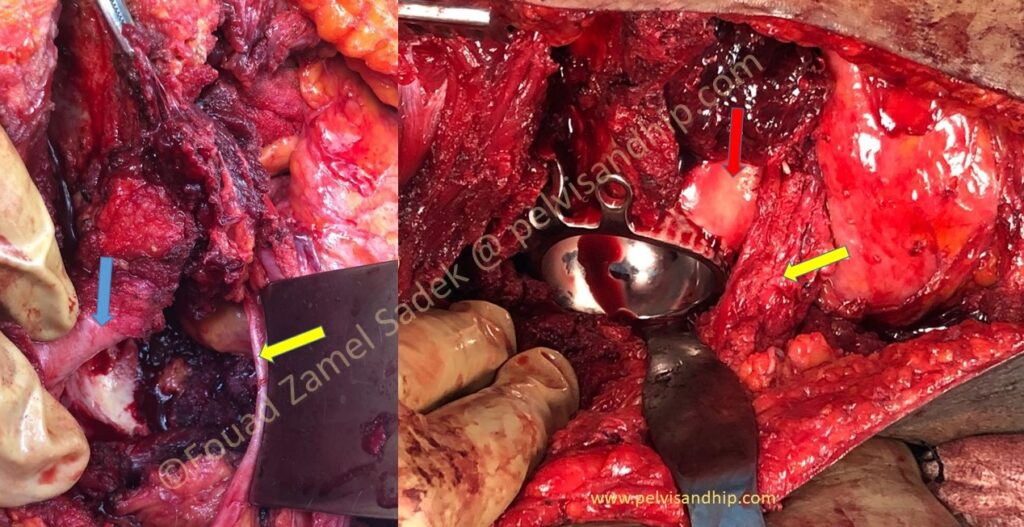
An Intraoperative picture (left side) of the bed of the right acetabulum after resection, one can identify the remaining posterior column and wall (arrow blue). One can appreciate the anterior and superior defect of the acetabulum, between the posterior column the external iliac vessels (yellow arrow). After application of a cementless dual mobility (right picture) cup with bone graft applied from her own femoral head; you can see the cartilage of the divided femoral head (red arrow). The femoral head and neck was divided with the cancellous bone part applied to the resection plane to obtain union after fixation with a reconstruction plate applied on the inner side of the ilium as the standard fixation done through the lateral window of an ilioinguinal approach.
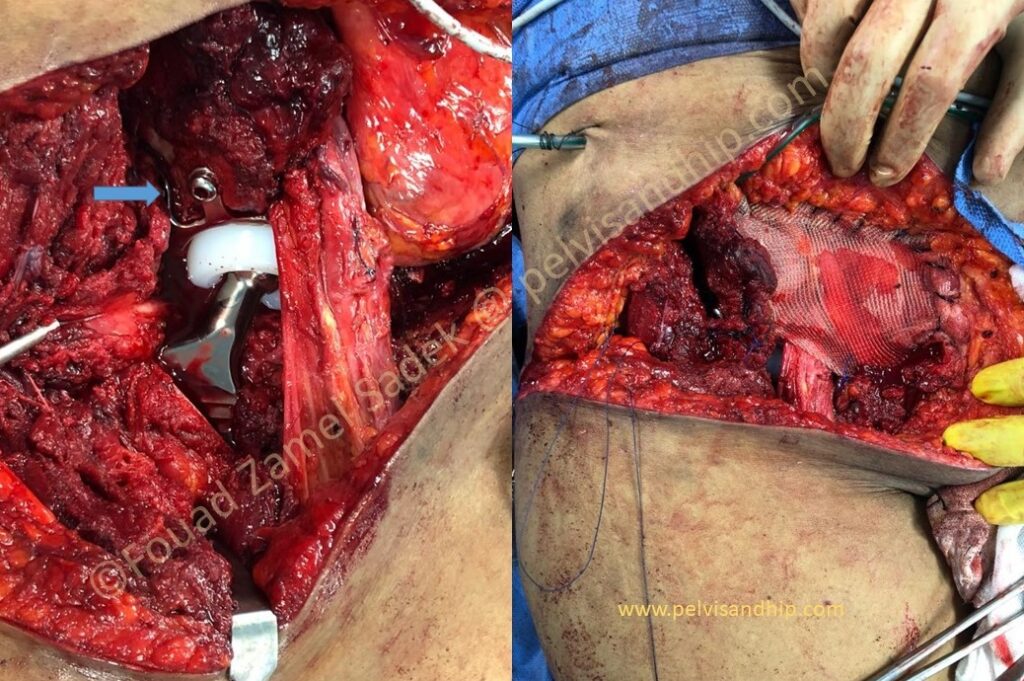
Through an extended transverse incision after the tumour resection, a cementless revision dual mobility hip was inserted. This was preceded with reaming the femoral head autograft to accommodate a press fit cup. Added screws were used through the flanges of the cementless shell (blue arrow). The cementless extended coated stem was inserted though the same technique used for stem insertion through a direct anterior approach with the hip in extension without the use of any special table. The stem can be clearly seen on the left picture with the cup and graft just posterior to the neurovascular bundle. On the right picture one can see the protective mesh applied around the vascular bundle before proceeding with further closure.

The size and extent of the skin incision can be appreciated in this picture with skin edges approximation prior to actual closure.
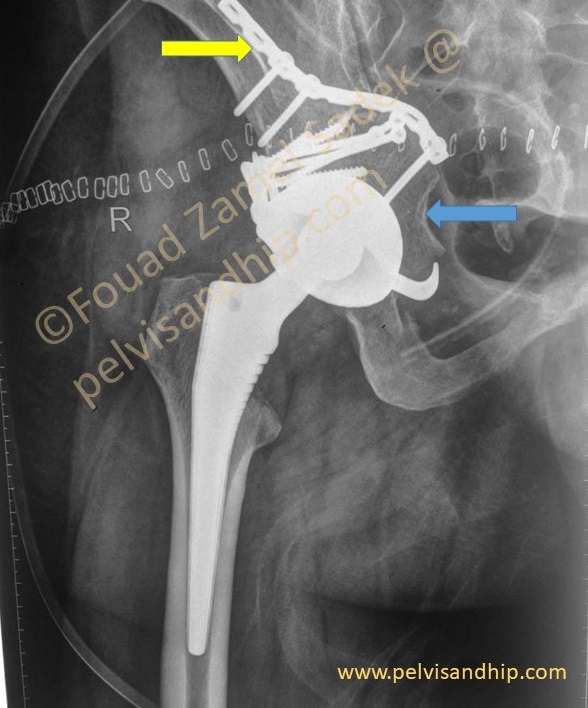
The final implantation of the cementless dual mobility can be seen. One can notice the femoral head and neck autograft (blue arrow) fixed with a reconstruction plate applied on the inner side of the ilium (yellow arrow).
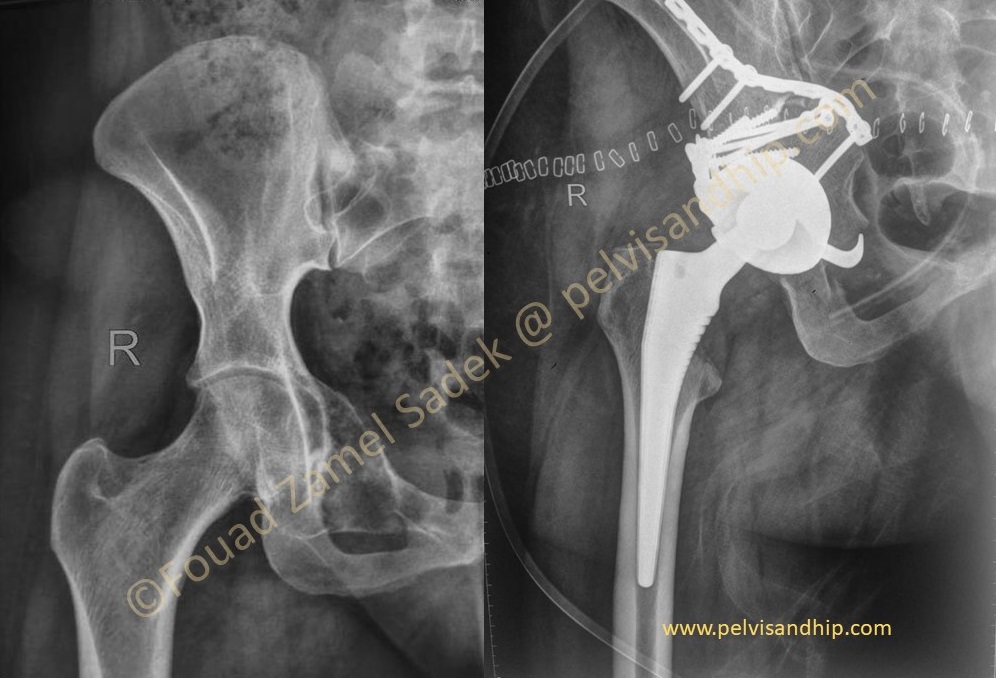
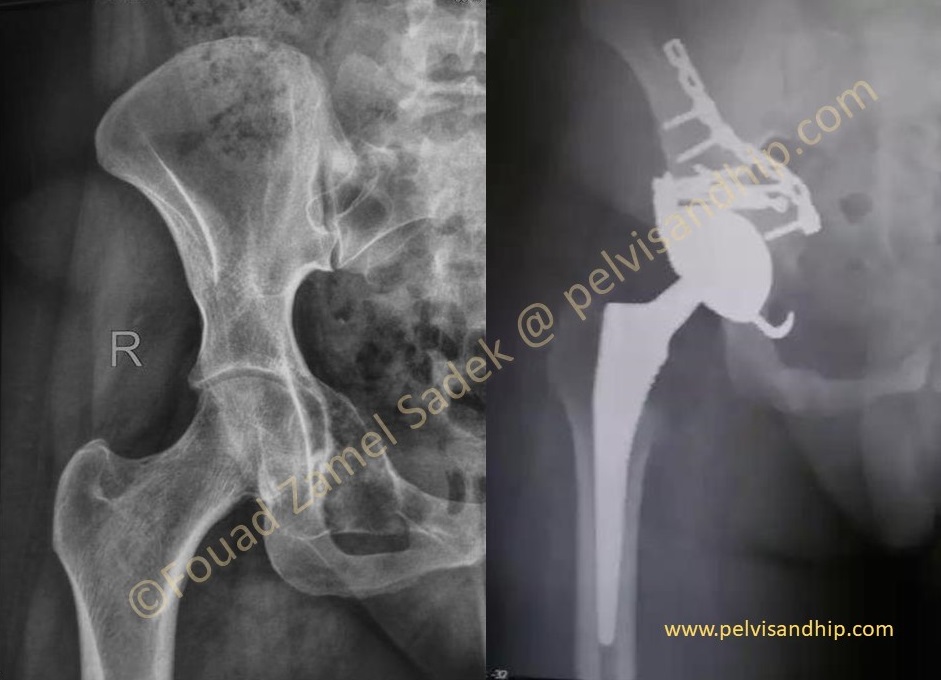
The preoperative x-rays prior to surgery side by side with the post reconstruction procedure with the hip replaced and the acetabulum grafted.

Follow up x-rays at 6 months with good osteointegration of the hip prosthesis and the close up view of the acetabulum confirms that the bone graft has survived with union and cup integration.

One year follow up with the patient walking full weight bearing with no support.
The learning points of this case: 1.Good preoperative planning is very essential to consider not only the resection procedure but also the options of reconstruction. 2.The transverse incision was quite versatile and allowed both resection and implantation. 3.Bulk femoral head autograft can be useful in such reconstruction as it tends to behave differently from bulk allograft. 4.A cementless dual mobility cup can be quite useful to provide stability considering the soft tissue resection. 5.Experience with the Direct anterior approach can be tailored and used for implantation of such cases with preservation of the posterior capsule and soft tissue envelope for better stability and better function. 6.Team work is the key to success in any complex case.

If you feel like posting comments, enquiries or questions please click here.