
If you also wish to view the author presenting this lecture you can click on the picture above. This was at the ITC in dubai 2019. Otherwise you can read the lecture downwards with the slides. Enjoy!
We all face delayed acetabular fractures whereby the initial surgical treatment was not carried out appropriately. This presentation is about a new way of linking acetabular fractures to resulting acetabular defects with a new philosophy of management
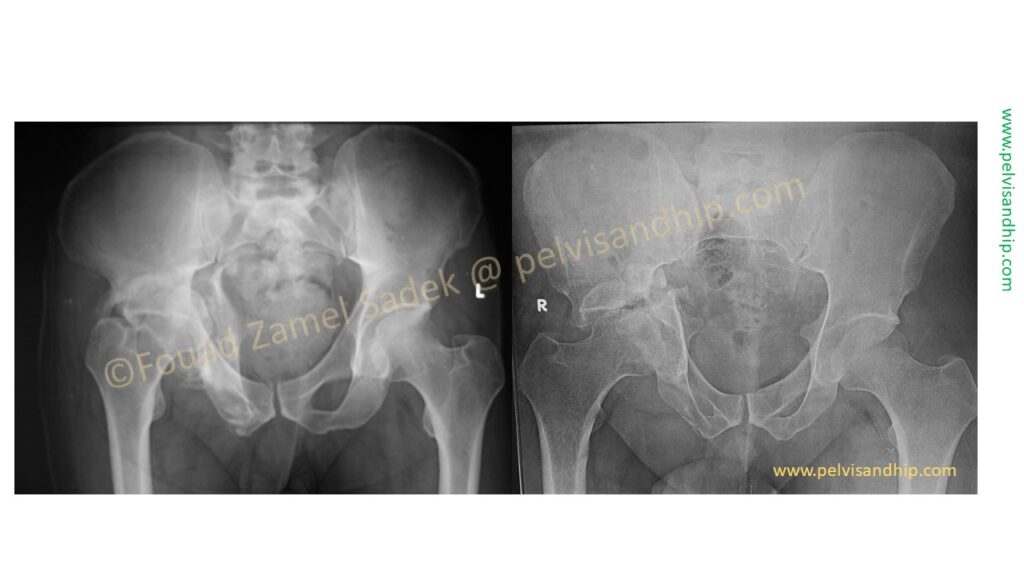
We all face delayed acetabular fractures whereby the initial surgical treatment was not carried out appropriately. There are cases whereby the displacement and therefore the resulting acetabular defect can be challenging but not all that challenging.
And there are cases which can be more and more challenging depending on how neglected the cases were.
The clinical presentations of acetabular fractures that need arthroplasty can be quite variable. There are fractures which were treated conservatively i.e without any previous surgical intervention. Those that had an adequate open reduction internal fixation procedure yet the results were not satisfactory whether due to avascular necrosis, osteoarthritis or any other complications that end up with an unsatisfactory functional result. There are those cases that had an inadequate previous fixation procedure. Lastly there are those cases whereby, recently there has been a trend for implanting an acute primary total hip arthroplasty, these are the cases associated with confounding variables causing an expected abysmal outcome. In such cases one would opt for an acute primary total hip arthroplasty to avoid a delay after an attempt of an internal fixation which is expected to fail anyway.
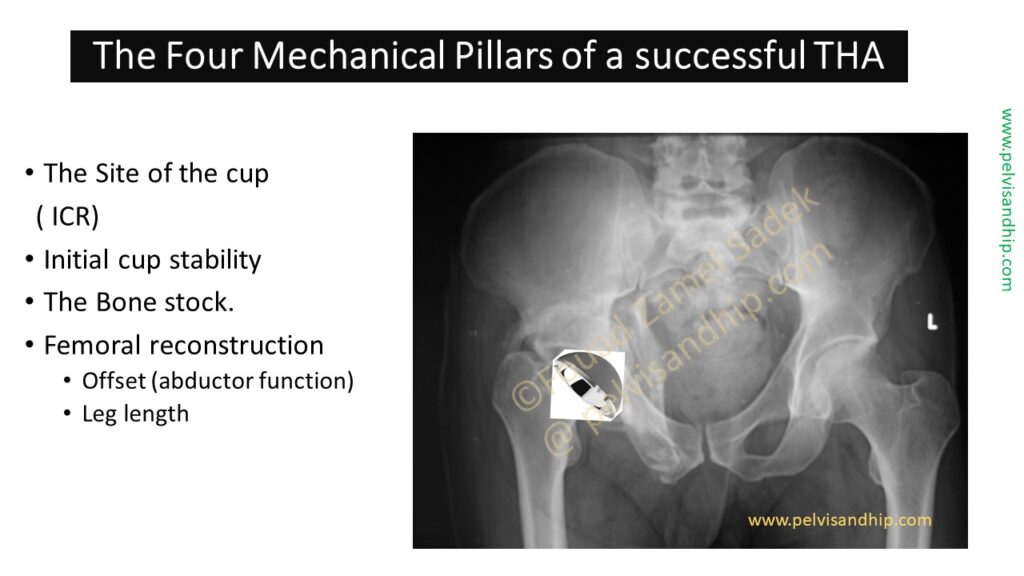
Like any complex reconstruction needed for any complex arthroplasty of the hip, reconsider the presence of four essential mechanical pillars for successful total hip arthroplasty procedure. The 1st and most important the site of the cup this has to go into at the instantaneous centre of rotation of the hip. Then the cup has to be put in the best place where there is a good bone stock to provide an initial cup stability. The last factor would be playing with the femoral reconstruction adjusting the offset for the best abductor function and the equalisation of the leg length.
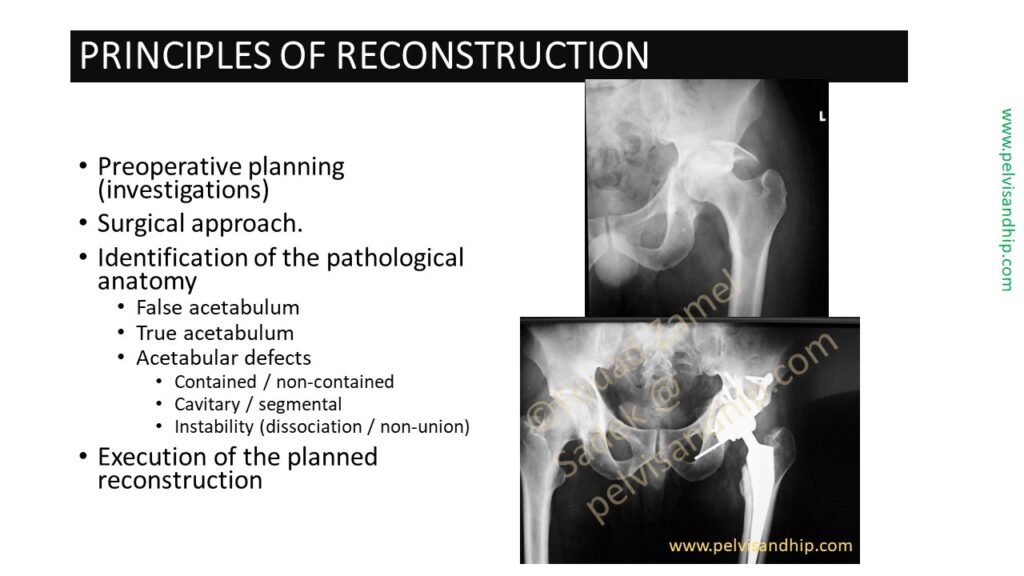
As part of your main preoperative planning obviously after considering the surgical approach, one needs to assess perfectly where the true acetabulum is and therefore considering the type of acetabular defect one has to deal with. The name of classification is not of paramount importance, as the issue is containment of the defect weather in cavitary or segmental position, and whether there is an added dissociation element probably due to a site of non union and on that basis the planned reconstruction can be formulated.
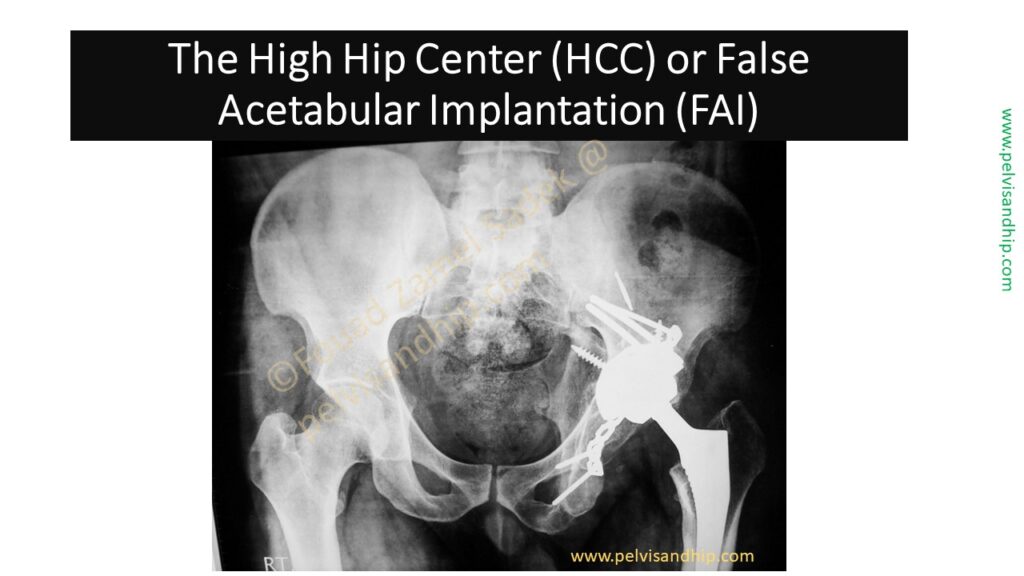
Planning will save you the hassle as well as the negative surprise of implanting a cup in high hip centre position or what we call a false acetabular implantation. We will not debate here the validity of a high hip centre versus the insertion at the true centre of rotation which we tend to prefer in our practise.
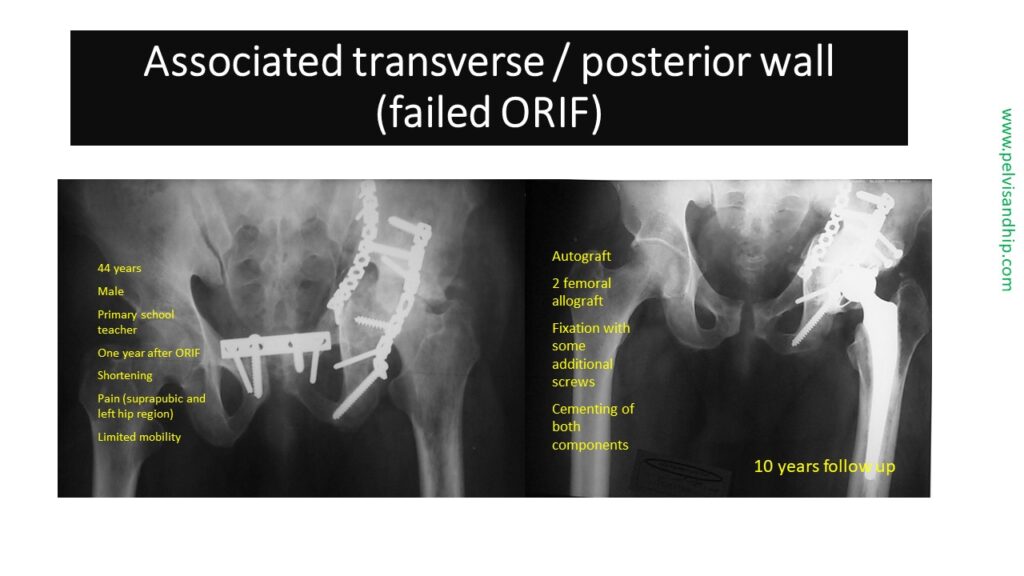
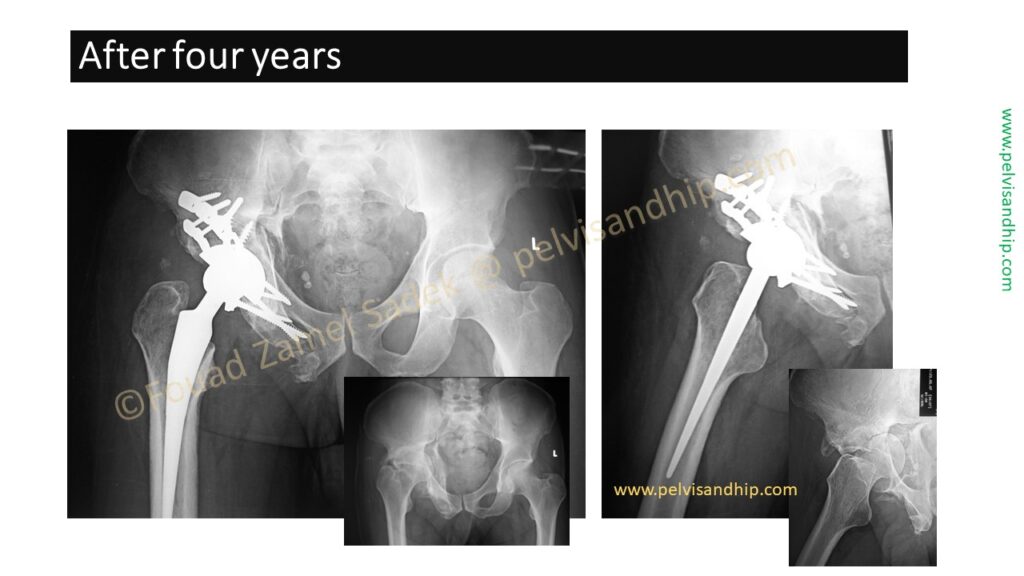
The previous old technique is presented well in this associated transverse with posterior wall fracture with a rather inadequate previously failed fixation procedure. This 44 year oldschool teacher presented to us one year after the previous fixation attempt with shortening pain in both the hip region and the supra pubic area and limited mobility. The reconstruction required the addition of two femoral allografts on top of his own femoral head with modification of the fixation using cemented implantation on both the stem and the cup which lies on top of an area of impaction grafting. The 10 year follow up vows to the validity of this reconstructive procedure.
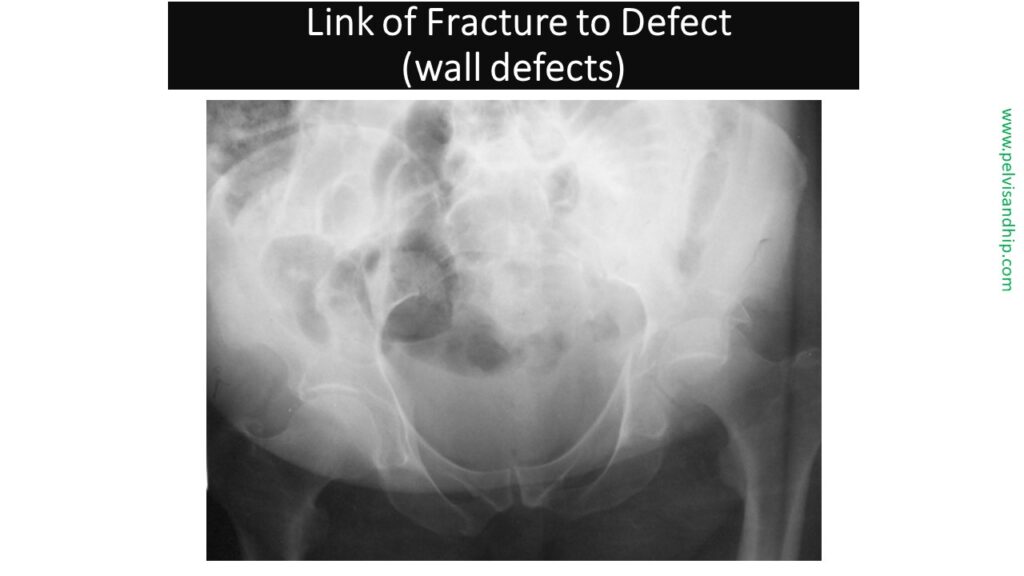
What has been lacking in the literature and practise is a link between the fracture type and the defect that results from these injuries. We are all familiar with different defect classification schemes mostly coming from arthroplasty surgeons with somewhat limited understanding and experience in fixation of acetabular fractures. The easiest to understand is the wall defect producing a simple segmental defect.
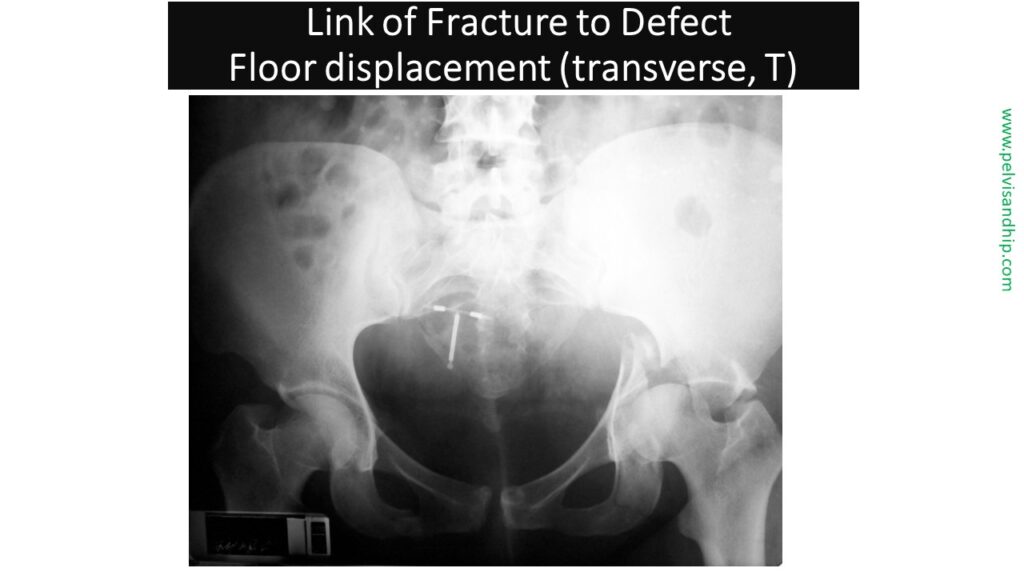
There are two different types of defects which are peculiar to an acetabular fracture. The first is what we call a floor displacement defect which results from a significant displacement of a transverse fracture or T fracture mostly involving the horizontal component of the T. In such a case the lateral part of the dome is rather complete and in place with loss of some of its components due to the inward displacement of the transverse fracture. In such a situation the surgeon has to decide weather to put the cup on the intact dome and build up the defects with the standard techniques of grafting and reconstruction or ream part of the dome to create one spherical socket, grafting the floor and enlarging the size of the cup in an attempt to work on the displaced fracture as it is.
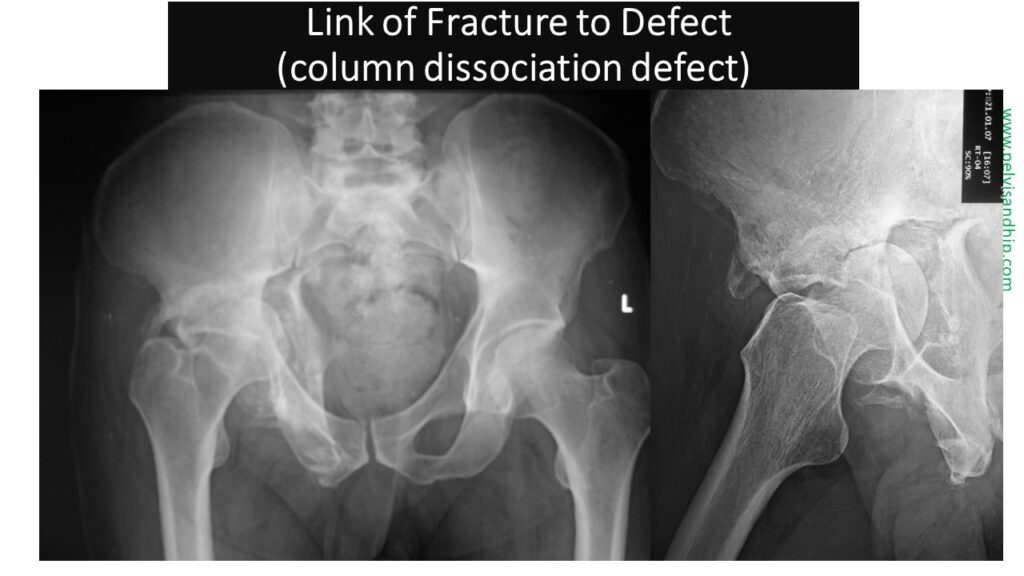
The last is what we call the column dissociation defect, very similar in principle to the defect resulting from the transverse fracture but in a vertical orientation. The column dissociation defect is when there is a single column fracture. The choice is between implanting the cup on the intact column and building up the defects from the displaced one or trying again to ream two columns together in one large space adding some graft to fill the gaps and enlarging the size of a cup. These two types can be treated by a totally different concept which is a delayed osteotomy of the fracture with reduction then fixation followed by implantation of the cup at the end.
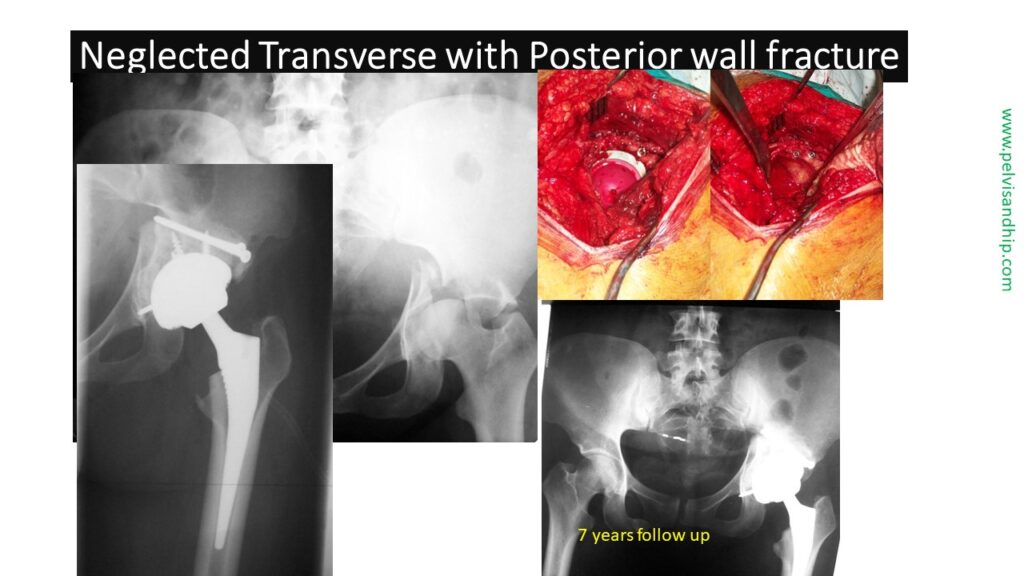
This neglected transverse with posterior wall fracture is the classical example of implanting a Cup without touching the displaced fracture. Upon union of this fracture, the cup was implanted after reaming the whole defect with part of the intact bone stock. Addition of bone graft from the patients own femoral head with fixation with two screws like the standards reconstruction was also done. In this case a cementless cup was press fitted in, with addition of some screws for initial stability. The seven years follow up vows to the validity of the procedure.
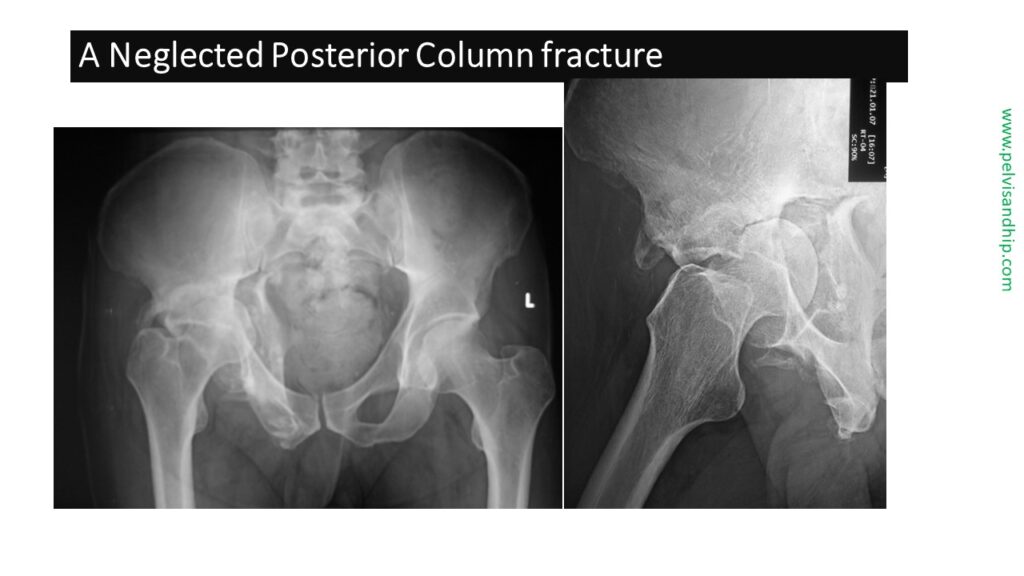
In this case a neglected posterior column fracture was dealt with according to this new concept of delayed osteotomy reconstruction and implantation. The posterior column in this case is significantly displaced and therefore it presents a challenge for cup implantation. After dislocation of the femoral head and the division of its neck, the access to the acetabulum becomes clear.
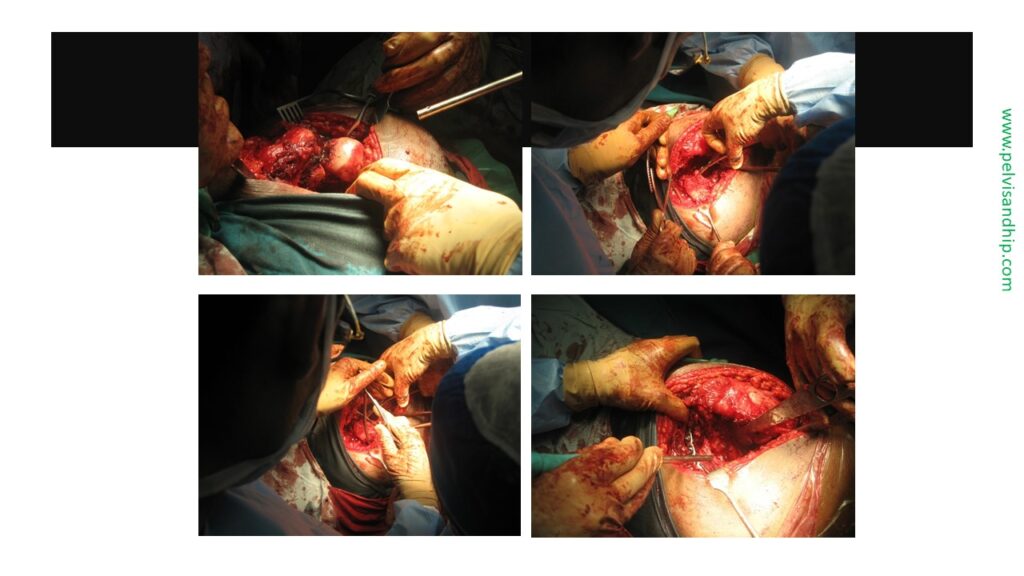
Full release of the fracture as well as the posterior column is done. A pointed reduction forceps was inserted with one arm into the lesser sciatic notch and the other in the Supra acetabular area with gradual approximation of the posterior column. Once the column was brought to its site, without aiming at an anatomical reduction, plate fixation was carried out.
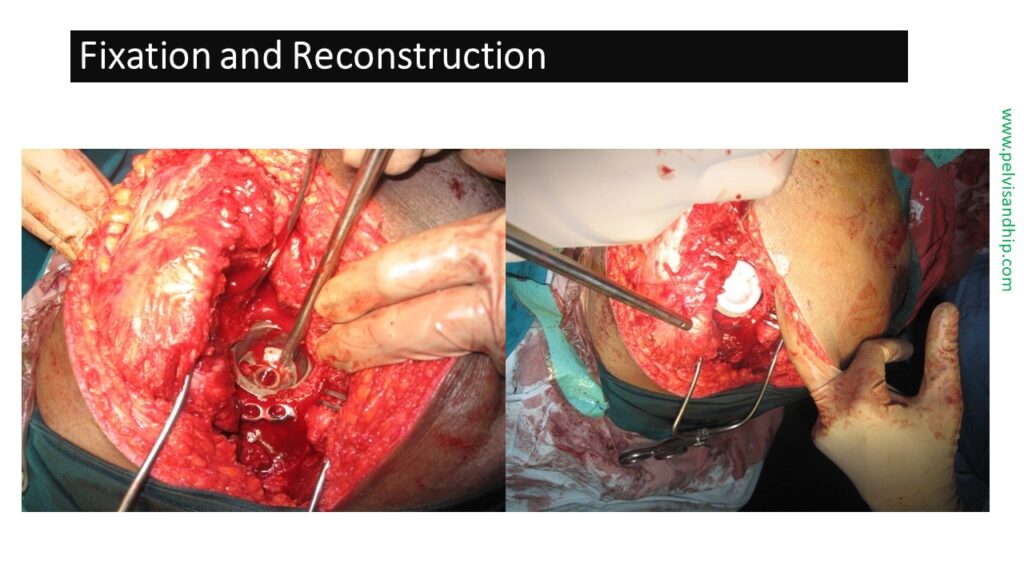
Acetabular reaming would make the bone stock suitable for the cup implantation, converting it into a spherical socket. In this case a cementless cup was inserted and press fitted with addition of screws for extra stability. A highly cross linked polyethylene was used.
A ceramic head was used. Two plates were used for the acetabular fixation for enhanced stability of this delayed fracture. One can appreciate the amount of reduction that was carried out between the preoperative status and the post reduction condition.

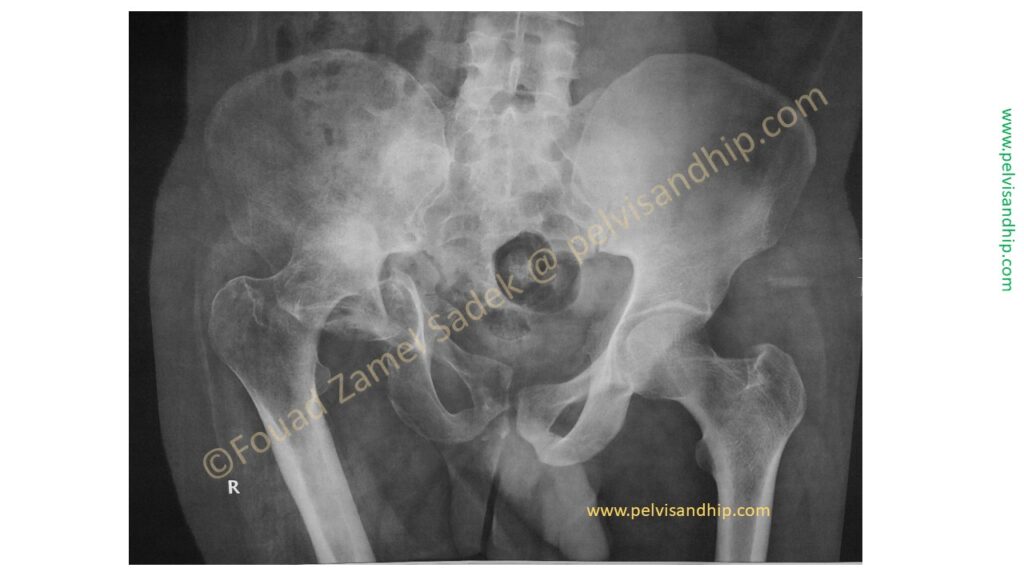
This accountant presented to us eight months after a road traffic accident. He suffered from a neglected transverse with posterior wall acetabular fracture. One can see the centrally displaced femoral head abutting against the dome which has been worn out; whether from the fracture or the articulation of the neglected femoral head against the fracture plane.

The oblique views further analyse the fracture. On the obturator oblique view the posterior wall can be seen in profile with appreciation of the posterior segmental defect that would result. The upward and medial displacement of the distal hemipelvis of the transverse component can also be appreciated with the gap between the remaining dome and the displaced hemipelvis.
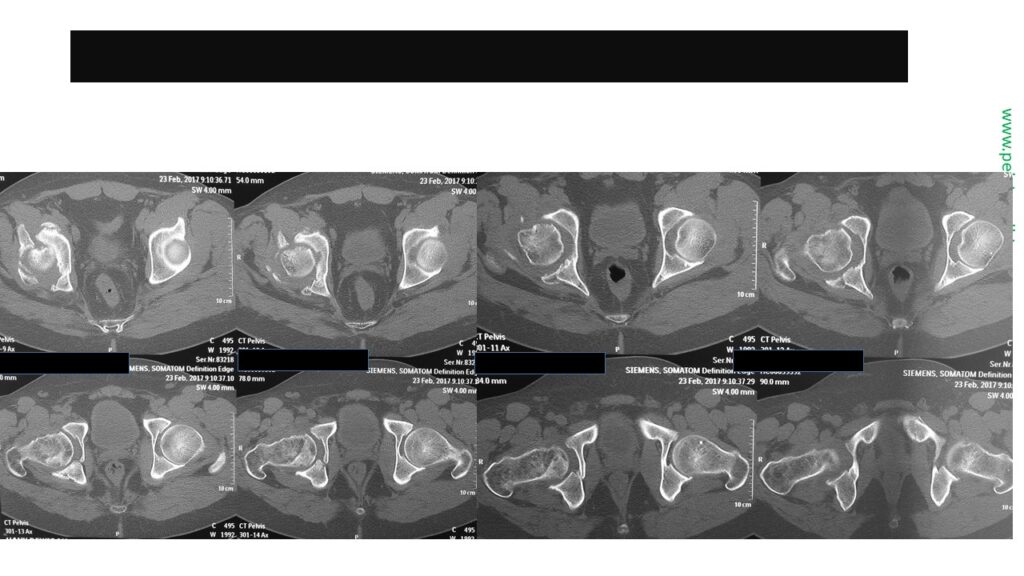
The axial cuts of the CT scan show the widening of the acetabular socket as well as the absence of a supportive posterior wall.
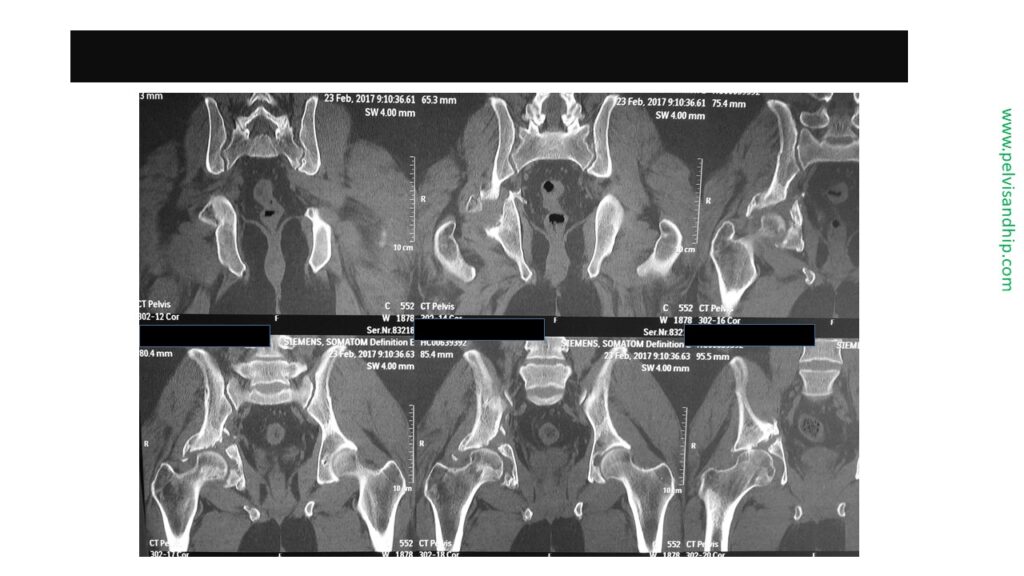
The coronal cut of the CT scan show quite clearly the non union of the fracture as well as the impingement of the femoral head on the fracture site with some deformity within the femoral head.
On the left hand side of the picture the coronal cuts show some area of attempted union which may need special techniques to mobilize the fracture. On the right hand side the posterior view of the 3D reconstruction clearly shows the medial displacement of the posterior column compared to the dome and the empty space of the fractured posterior wall.
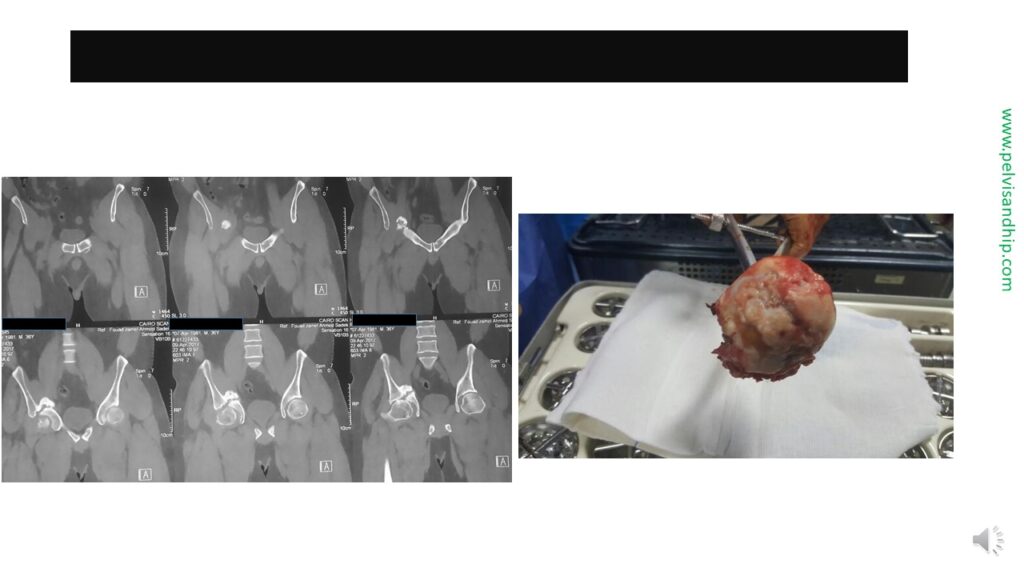
The picture of the femoral head reveals that it was damaged and thereby a delayed reconstruction without replacement would not work.

Cementless implantation was done after the delayed osteotomy of the transverse fracture and its mobilisation. The fracture was fixed with plate and screws. A press fitted cementless cup was inserted with added screws for extra stability. Any remaining small defects were filled with his own femoral head as an autograft.

The iliac oblique view shows the good seating of the Cup after the delayed reduction of the fracture.
Other views shows the good seating of the Cup and the good bone support with a satisfactory reconstruction.
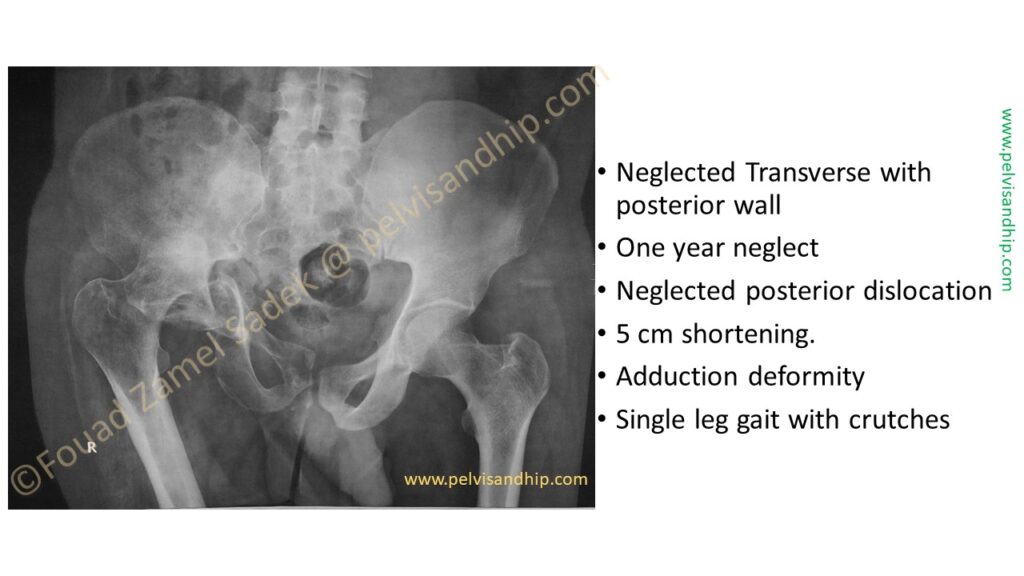
This a somewhat more challenging case presented to us one year after a neglected transverse fracture with a posterior wall. The 25 years old, young man who was exposed to this injury could only walk with a single leg gate, with crutches, having five centimetres shortening and a significant adduction deformity.

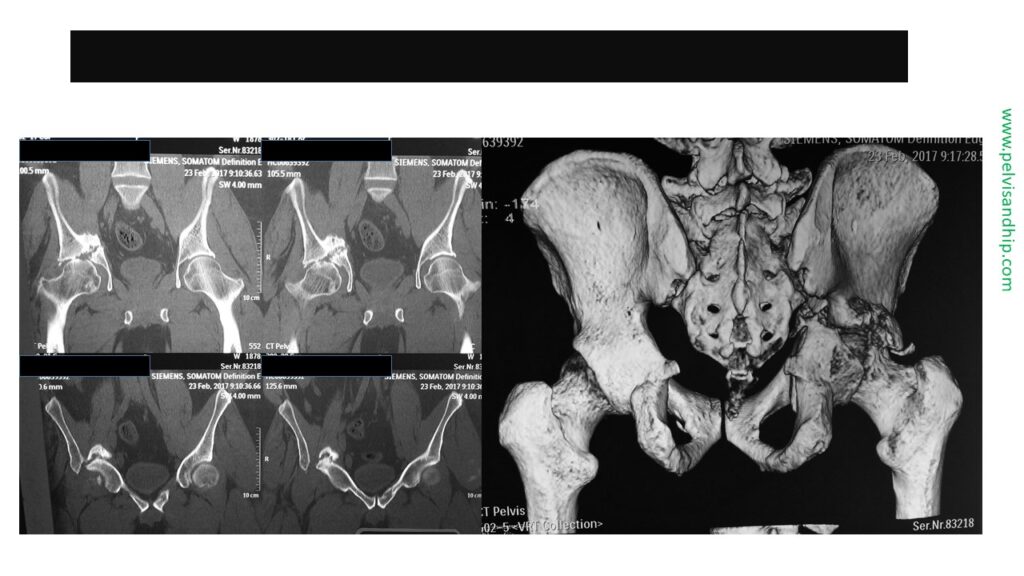
There is a neglected posterior hip dislocation. The distal hemipelvis is significantly displaced inwards and upwards. On the 3D reconstruction one can see a posterior wall residing within the dome space and the femur is in significant flexion adduction deformity.

A more clear representation of the pathology seen on the 3D reconstruction. You can see the posterior wall within the acetabulum, the femoral head posteriorly and superior displaced, as well as the flexion adduction deformity of the hip.

The posterior view of the 3D reconstruction on the left hand side clarifying the position of the femoral head. The lateral view of the 3D deconstruction is also clear.
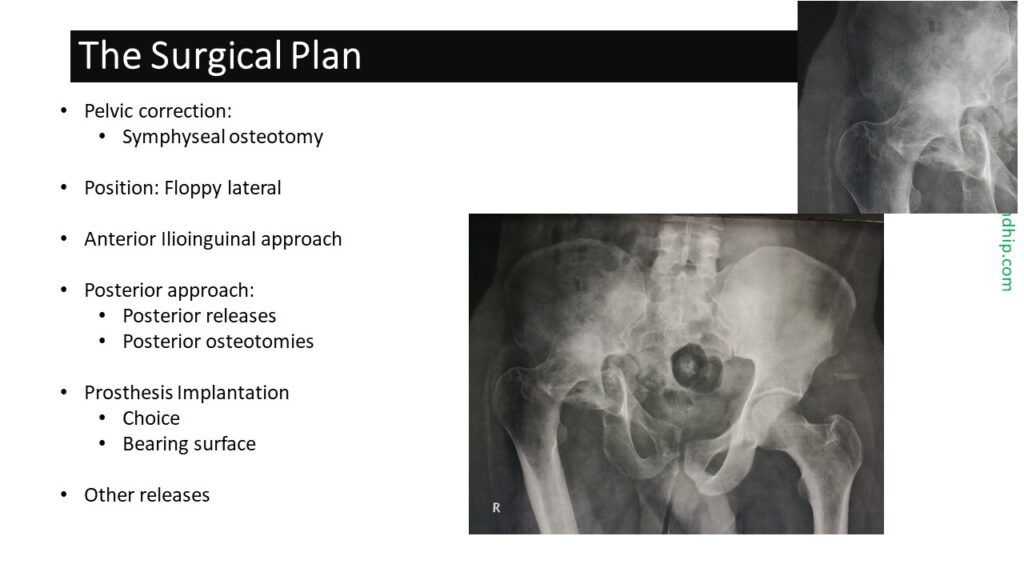
The full evaluation of the fracture shows that this is indeed an associated pelvic and acetabular fracture which means the pelvic fracture is contributing to the deformity and displacement. To mobilize the acetabular fracture one has to consider the displaced pelvic component. For this the first step would be symphyseal osteotomy and its mobilization, not aiming at reduction and fixation. The position is what we call a floppy lateral position, to allow both access with an anterior ilioinguinal approach combined with the posterior approach for the releases and osteotomies. A satisfactory reduction and fixation will provide good bone stock for prosthesis implantation.

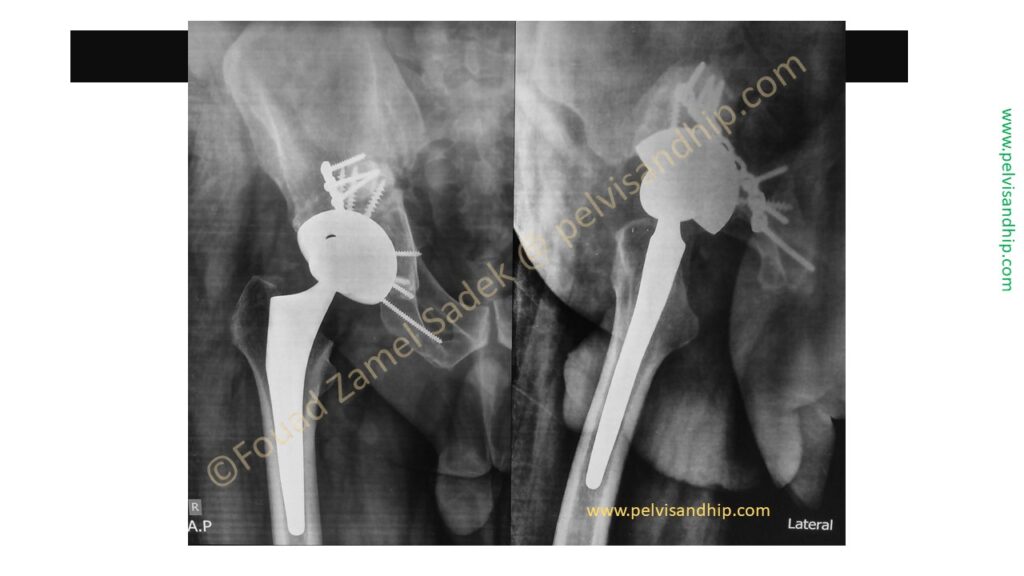
After complete releases both anteriorly and posteriorly for the symphysis as well as the acetabulum. The fractures were reduced and fixed with an anterior plate and a posterior plate. The femoral head was used for autografting for the neglected posterior wall component. Cementless implantation was carried out with a ceramic head on highly crosslinked polyethylene.
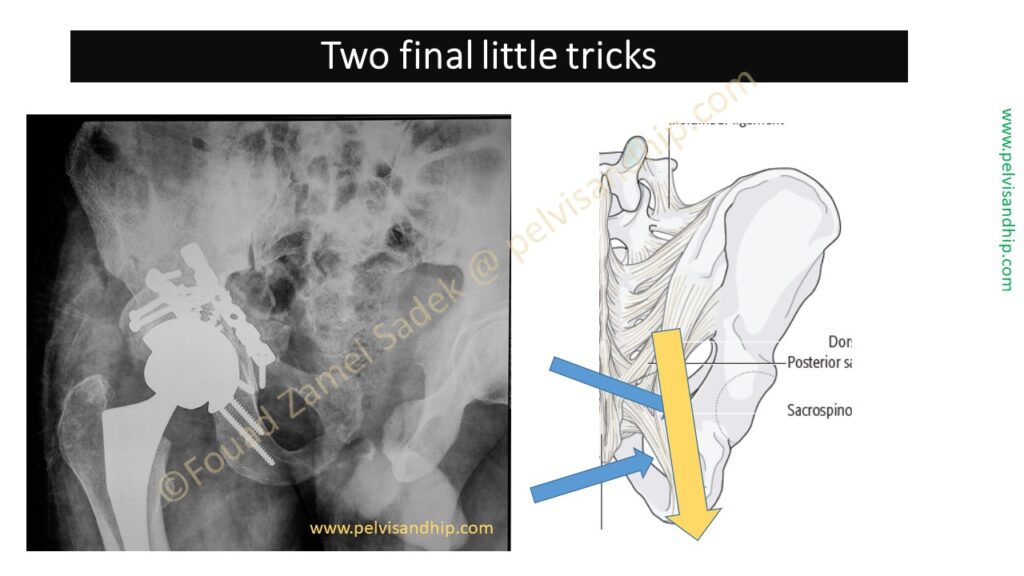
Adequate releases are the key to success, aiming at the sacrospinous and sacrotuberous ligaments which have to be released in sequence. The base of the spinous process is osteotomized first to avoid the pudendal vessels which will provide some release for the posterior column. The latter will be held by the sacrotuberous ligament alone. This is usually covered by the sciatic nerve as shown by the yellow arrow which needs to be gently mobilised medially to gain access to the ligament. The latter is divided with scissors slipped underneath the sciatic nerve close to the ischial tuberosity dividing the ligament fully. Once this is achieved the full mobilisation of the posterior column becomes easy. Such reconstruction requires meticulous attention to detail but it provides quite satisfactory bone stock for cementless cup implantation at the site of instantaneous centre of rotation of the hip.
The take home message of this presentation is that the standard acetabular defect classifications for arthroplasty implantation needs to be modified in the light of the peculiar acetabular fractures. A delayed reduction with an osteotomy of the healed fracture together with internal fixation provides a good reconstruction for a cementless implantation. Surgeons trained in both pelvic trauma and arthroplasty are most suited for this procedure. Thank you for listening.