

37 years old banker, who had a road traffic accident after which he had a right acetabular fracture associated with a partial sciatic nerve injury. Orthopaedic surgeon who initially managed him opted for open reduction and internal fixation with dual approach both front and back. 7 months down the line he has a delayed dislocation which was deemed to be due to avascular necrosis. Initial treating surgeon did this total hip implantation with what looks like a reversed hybrid reconstruction.
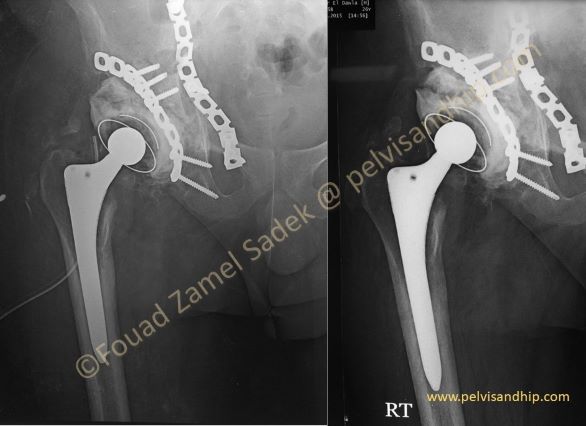
3 months down the line he is starting to suffer from pain with a history suggestive of infection with several attempts of washout with persistence of infection with intermittent discharge.

A few months later, he presents to the hospital with loosening of the acetabular component and severe pain with inability to bear weight in the right lower limb.
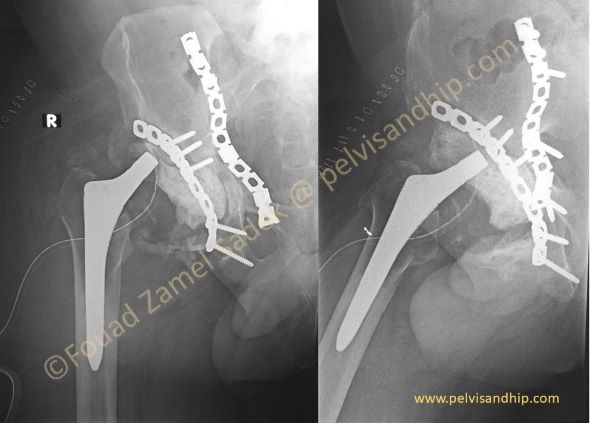
Initial treating surgeon opted for a staged revision but for some reason attempted to choose a single component revision for infection (which is a rather debatable policy). The story is that he removed the loose acetabular component with its cement through a posterior approach without removal of either the stem or the plate. The operative history states that the stem was found to be very stable which is expected about a year after having had the stem implantation.

Persistence of infection with elevation of all inflammatory markers including CRP and ESR together with persistence of pain after which the patient was referred to us. The decision was that he definitely needed to have both the stem as well as the metal work removed to ensure clearance of infection. The preoperative culture was positive for MRSA. After removal of the stem one could recognize the special cementless design of the stem with extended proximal coating with titanium mesh for ingrowth as well as grit blasting of the middle part of the stem for ongrowth. Note the well integrated growth of bone on the surface of the stem.
One can see on this video how well the bone ingrowth/ongrowth on both titanium mesh as well as the grit blasted component of the stem. Introperatively, one could lift the stem holding the remnants of bone integration. (please click on video)

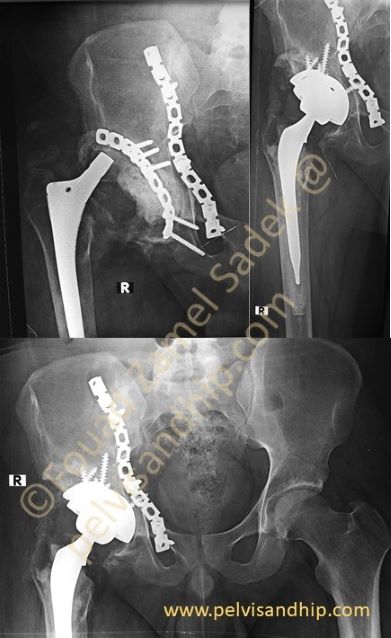
After another 2 months the second stage was carried out as per routine with the use of a reverse hybrid reconstruction. The acetabulum had a superoposterior defect which was reconstructed with a trabecular metal augment and a cementless cup using a ceramic on highly-cross polyethylene liner.

AP and lateral views of the reconstruction at 3 years follow up. Patient had recovered his full hip function and returned to work. His sciatic nerve function also recovered with satisfactory discharge for long term follow up as per routine.
Learning points: 1.Infection needs vigilant management and walking the extra mild both for diagnosis and management. 2.Once suspected one should strive to ensure diagnosis. 3.Clearance of infection requires aggressive management with removal of potentially infected metal work even well integrated stems and difficult to remove posterior plates. 4.Understanding the implant design helps in planning not only insertion but removal as well. In this case an endofemoral approach for removal. 5.In young patients we prefer to try to use short stems in revision leaving the femur for future revisions if needed and sparing longer stems. 6.Trabecular metal augments are useful implants for quick acetabular reconstructions.