

26 years young man exposed to a severe road traffic accident where he was run over by a bus. He was admitted to ER in our pelvic unit with shock, and suspected for intraabdominal injury for which he went to emergency exploration. He also had a severe head injury that needed surgery for extradural haemorrhage. He also had a severe perineal soft tissue injury. Ended up later with a diverting colostomy and a suprapubic cystostomy, after his abdominal exploration.
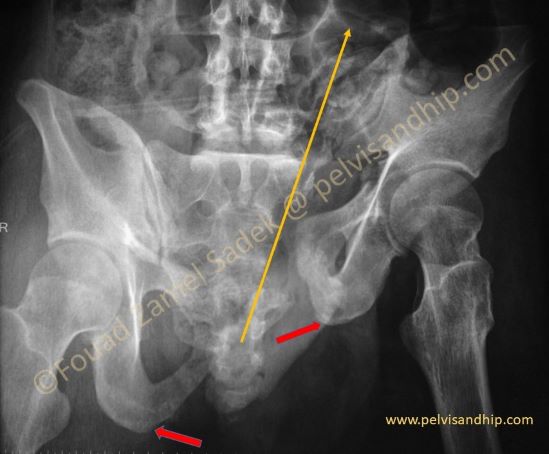
The pelvic views are very clear regarding this vertical shear injury. These significantly displaced injuries mount to what we tend to call them internal hemipelvectomy injuries. The injured hemipelvis is totally separated from the axial skeleton with total disruption of all soft tissues probably saving the neurovascular and some of the main internal organs. The plane of the injury is depicted by the long yellow arrow. Note the significant discrepancy of the two ischial tuberosities (two red arrows). The sacral injury is a Dennis type II to III, going through the sacral foramina.

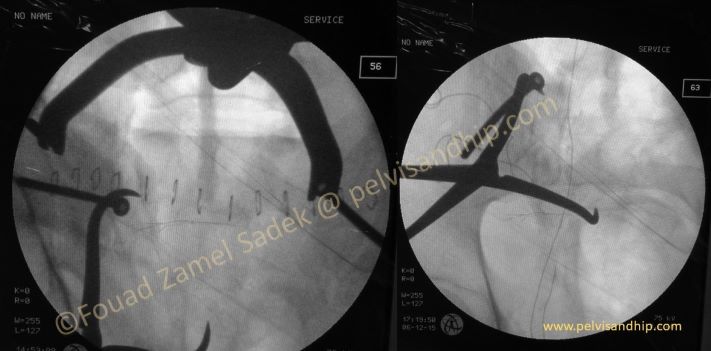
As part of damage control surgeries, on admission the initial treating surgeons applied this form of external fixator to stabilize this very unstable injury.

The damage control external fixator did not improve much of the vertically displaced fracture but probably contributed to the attempt of general stabilization of the patient.

Patient was admitted to the intensive care unit and needed to stay there for more than 8 weeks, for various interventions and follow ups, including not only his perineal soft tissue wounds and abdominal interventions, but more importantly his neurosurgical injuries and its sequalea, including interventions for management of shunts. One of the conditions he ended up with was Diabetes insipidus which required a very vigilant fluid and electrolyte balance management.
Patients more often than not loose their contact with one treating surgical team and once in the ICU’s; they seem like they get on a “roller coaster” whereby once you start the ride you have to take it all the way until the end and then their presentation for definitive interventions becomes significantly delayed.

3 months after the injury, our patient was bedridden presenting with significant shortening with inability to walk let along stand. The left lower limb in external rotation deformity. His perineal wounds had healed with a foot drop. He has significantly distorted flanks. He is also suffering from Diabetes insipidius.
There were different issues at hand with this 3 months late presentation. The first was to operate or not to operate. If we are to embark on an extensive reconstructive surgery what was the aim? What sort of surgical approaches were to be chosen? What would be the sequence of the procedures. How to get the appropriate reduction and what methods of fixation were going to be used? Obviously, we have to anticipate a high level of complications that we are to explain to patient and relatives. Anticipating all sort of risks involved the decision was to proceed for this severe injury incompatible with any life form.

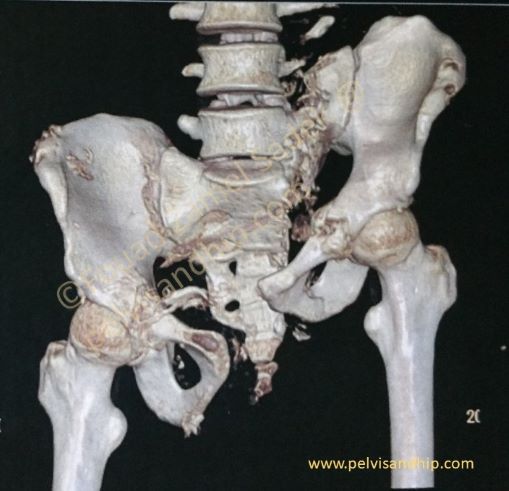
The 2 inlet and outlet 3D views show with great clarity the severe injury. Our usual protocols for management of neglected pelvic injuries especially the vertically displaced ones is to have some sort of a triple attack; whether front, back then front again or the other sequence around. Usually the middle stage would be the one where the reduction is finished and fixation started as the first stage usually entails some form release followed by partial mobilization or partial reduction with no fixation unless the latter would have no effect on the second stage reduction. The final or third stage is usually consisting of fine reduction tuning and adjustment associated with the completion of fixation

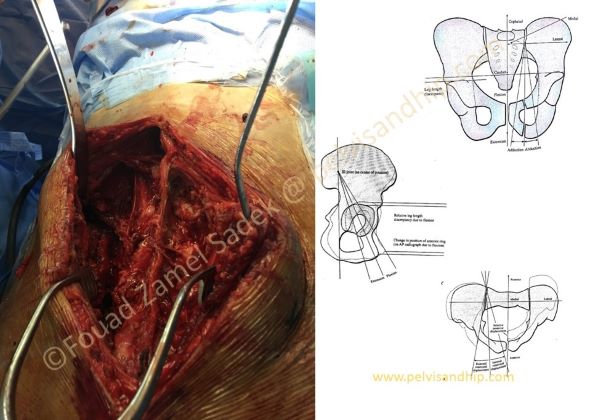
First stage anterior release: The surgical plan here consisted of an anterior approach first with exposure of the symphyseal area and complete release of all scars and soft tissues filling the gaps between the two pubic bones going as far laterally as possible. Such an exposure is usually done by a transverse pfannestiel incision. In other neglected injuries this approach allows more rotational control than vertical displacement and other dislocations. No attempt here was carried out for any fixation lest it interferes with other reduction manoeuvres.
Second stage posterior release and second reduction manoeuvres:
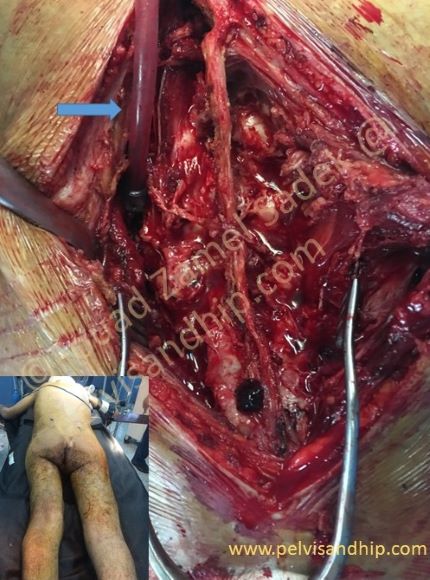
Patient is turned to the prone position whereby he is approached through a direct longitudinal approach as per other spine procedures. The sacral fracture is exposed in this position as it is on the left side of the picture. Note the plastic sucker (blue arrow) inserted in the fracture gap after its release and exposure. The dissection with this approach is taken by elevation of the paravertebral muscles from the midline laterally contrary to other standard approaches done for pelvic ring injuries whereby we tend to dissect the muscles from lateral to medial.
Second stage posterior release and reduction:
After the fracture has been fully exposed proximally to distally, we have to reach the most lateral edge of the sacrum sometimes distal the sacro-coccygeal junction. Both the sacrotuberous and sacrospinous ligaments are released fully from this posterior approach by enmass elevation of all soft tissues including ligaments and healing scar tissues from the lateral edge of the sacrum. Further releases are done from the medial aspect of the iliac tuberosity posteriorly. The last particularly difficult to reach structure, is the quadratus lumborum and paravertebral muscle fascial attachment along the iliac crest from posterior as far anteriorly as possible sometimes reaching the iliac tubercles on the anterior half of the iliac crest.
Second stage posterior release and reduction:
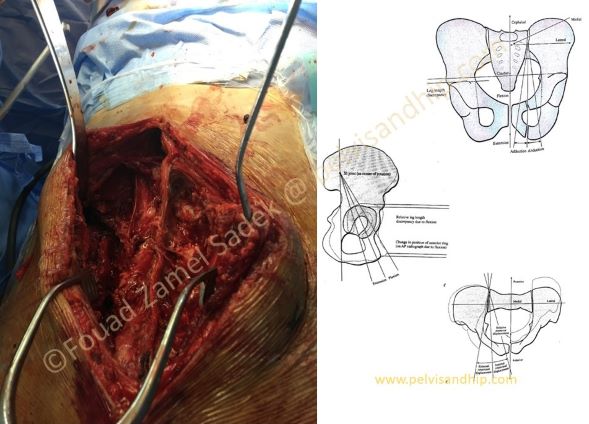
When these very tough ligaments and fasciae are not released, their shortening and contractures caused by the neglected injuries with vertical displacement can significantly hamper our attempts to bring down the displaced hemipelvis. The diagrams on the right explain the 6 different directions of displacement that the displaced hemipelvis has in the 3 dimensional space. A clear understanding of these directions of displacement is mandatory to be able to reduce the injury correctly by reversing the direction of displacement to bring down the pelvis to its anatomical position.
Second stage posterior release and reduction:
After the extensive releases mentioned above, reduction can be attempted and we advise surgeons never to start reduction prior to this complete and aggressive releases as they will be disheartened and doubt expectations for adequate reduction. There are different tips and tricks that one can use in anchorage and reducing the pelvis; the most versatile and used one is the large pelvic reduction clamp with screws with one screw applied in each iliac tuberosity.
Second stage posterior release and reduction:
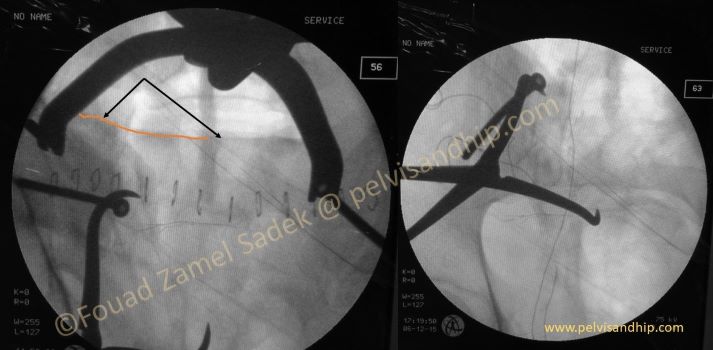
Another very simple yet highly effective manoeuvre is to apply a pointed reduction forces on across the sacral spines distally which have usually good bone purchase; the second arm can be applied across on long screw head inserted into the iliac crest so that the bone does not cut through. You can notice here the full reduction achieved (arrows) pointing to the upper border of the first sacral body (yellow curve). On the inlet view you can appreciate the successful reduction of the anterior border of the sacrum as well with alignment with the SI joint.

Third stage; anterior reduction and fixation:
In this particular case it was obvious to us that after the second stage there was still residual reduction steps to be taken on the anterior approach afterwards. For this we postponed the posterior fixation and patient was turned over again on his back to reduce the rotational displacement of the pelvis and fix the symphysis with an anterior 3.5mm reconstruction plate with strategically placed screws criss-crossing inside the pubic bones for best purchase. One can notice that there is residual pelvis flexion/extension mismatch causing the unequal appearances of the obturator formina at the end of this stage (circles)

Fourth stage: posterior reduction and final fixation;
Patient was turned over one last time in the prone position and this time the clamps of the posterior reduction (second stage were reapplied) correcting this last mismatch and the symphysis appear now better reduced. This is a procedure that is helped by the use of the 3.5mm reconstruction plate that allows bending of plate along the H direction by the reduction of the posterior pelvis.
Fourth stage posterior reduction and final fixation:
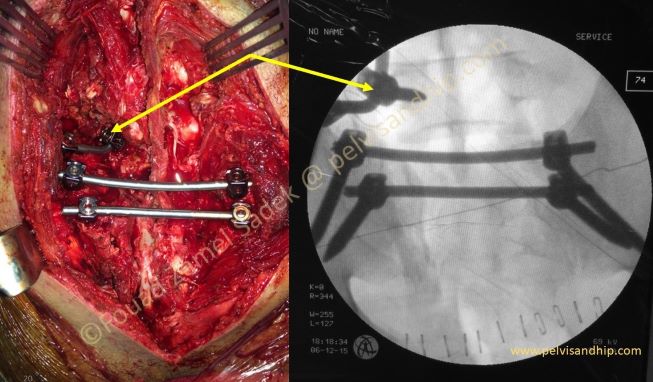
The posterior sacral fracture was reduced a second time with fixation using spinal stabilization systems. The first one is using double rods with fixation between the two iliac tuberosities. One extra spinopelvic application (yellow arrows) was added for extra stability considering the huge force applied to ensure reduction of such a neglected case (surgery was done 3 months after injury). One can appreciate the alignment of both SI joint areas and the satisfactory sacral reduction and fixation.

The final postoperative picture reveals the full reduction and fixation with satisfactory posterior ring reconstruction with some mild residual displacement of the anterior ring; which we were ready to accept. Notice the two approaches the longitudinal posterior clips of the posterior approach and the transverse pfannestiel anterior approach as well.

The outlet view shows clearly the good posterior reduction. The criss-cross screw insertions of the anterior symphyseal plate which is our current recommendation for anterior ring fixation in any case as much as we can. This is one of the reasons whey we prefer to use 3.5 mm screws in anterior fixations.

The inlet view also shows the well reduced left sacral fracture which completes the ring satisfactorily both posteriorly and anteriorly.

The final picture shows the amount of reduction that was needed to fix this pelvic injury from significant vertical displacement to satisfactory reduction and fixation.

The Learning points: 1.Careful planning is one of the most important issues not only in such complex and neglected cases but in any surgical intervention. 2.With any interventions one should have a well defined set of goals aimed at by the procedure considering all the possible complications and risks. 3.One of the main key points of decisions is the sequence of surgical exposures. For most neglected pelvic injuries more than one exposure is usually needed and one must have a clear understanding of what each surgical approach would achieve and how to go around reaching each goal in terms of reduction and fixation. 4.Each step of the surgery has to be carried out meticulously and carefully not proceeding to the next step until the goals of each step have been reached successfully. 5.The final word of advise is to manage patient from the start and try to avoid them become neglected with delayed presentations; don’t let them go on the roller coaster.

If you feel like posting comments, enquiries or questions please click here.