
33 years male who works as an air hostess. Presented to me for a left acetabular fracture. He states that he has been having left hip pain for more than 2 months and just one day before he had a simple fall on the ground after which he had severe pain and he was unable to bear weight. Transferred to hospital with no other associated injuries. Neurovascaularly intact.
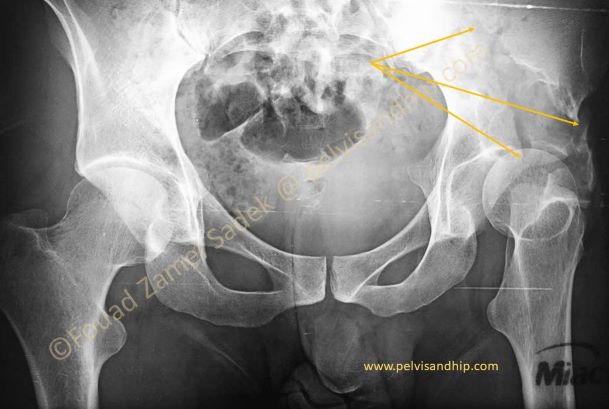
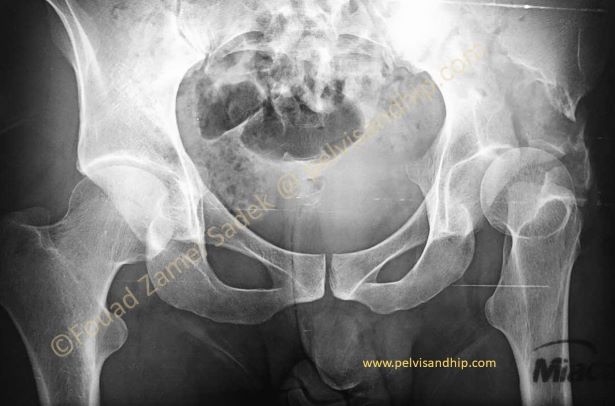
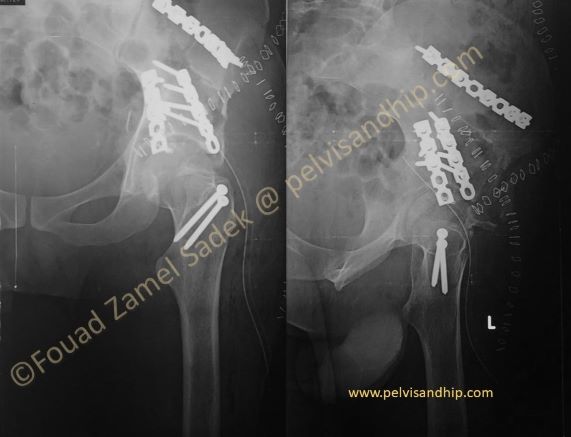
On the AP view of the pelvis, there is a fracture of the left acetabulum which is rather difficult to classify; sort of looking like a high anterior column fracture. This is on top of a huge osteolytic lesion with different ill defined and well defined edges. The hip is in a position of extreme lateral rotation making the view similar to a lateral views of the hip. There is a somewhat subluxation/dislocation laterally following the fracture column.

On the iliac oblique view the intact posterior column is confirmed. The fracture involving the anterior column is also well demonstrated. The large size of the osteolytic lesion can be depicted clearly. There is an extra fracture fragment which seems to be involving the anterior wall of the acetabulum as well (blue arrow).
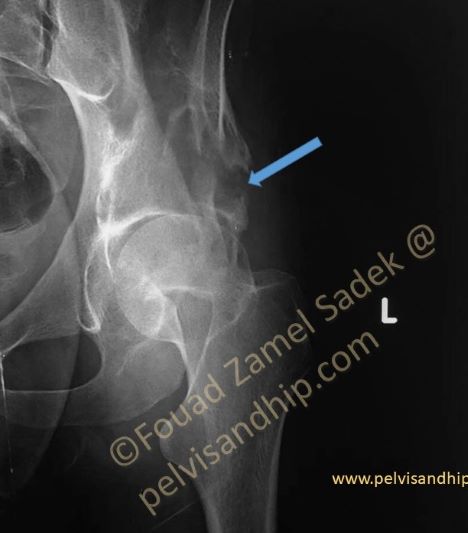
The obturator oblique view shows the intact standard iliopectineal line which is more in accordance of a special fracture pattern, either a very high anterior fracture or a dome like fracture (blue arrow) with some proximal extension. The posterior wall line is rather intact.
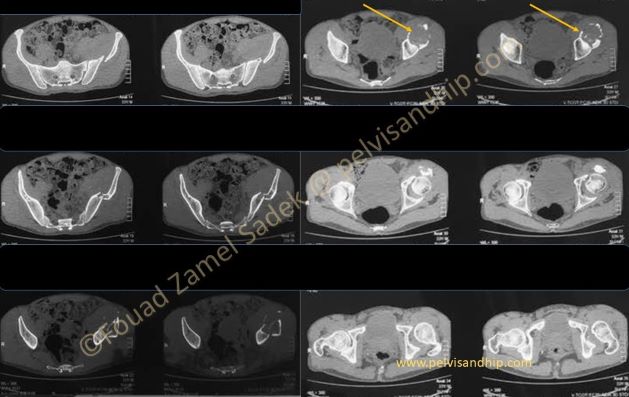
The axial cuts of the CT scan confirm the very high anterior column fracture with involvement of the anterior part of the dome including the osteolytic lesion of the ilium (yellow arrows)
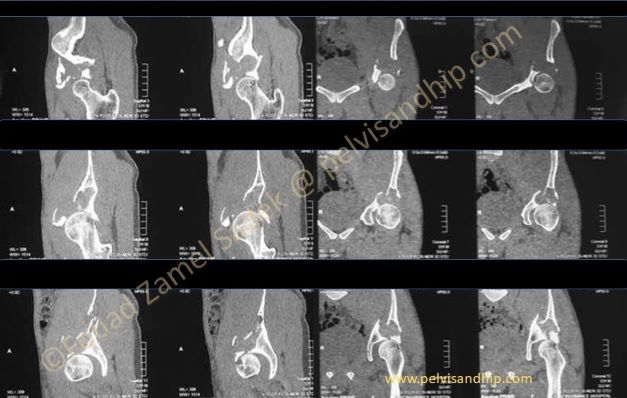
The sagittal and coronal cuts clarify the extension of the osteolytic lesion with involvement of the dome. The fracture can also be identified within the walls of the lesion.
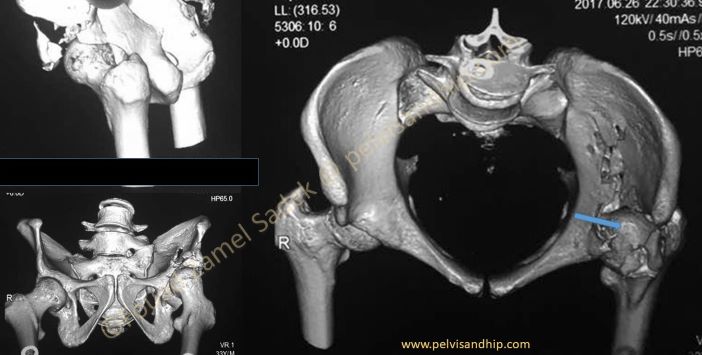
The 3D views do not really show the extent of the osteolytic lesion but this is expected being a surface rendered imaging but it helps to identify the high anterior column fracture and one can see the femoral head uncovered with a rather superior wall fracture on top. (blue arrow)
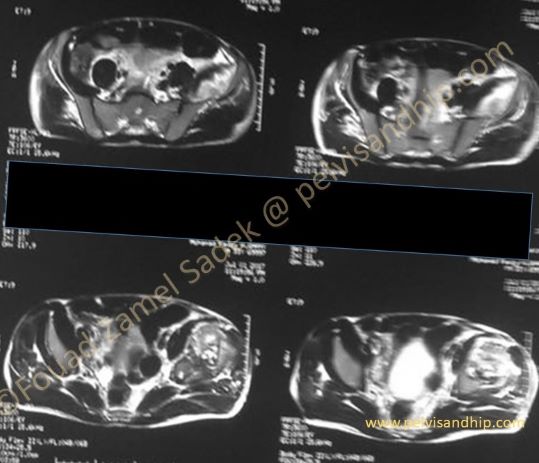
MRI investigation of the case shows a large cystic lesion with fluid admixed soft tissue components within the osteolytic lesion.
So we were faced with a double problem; the first and most obvious the acetabular fracture with significant damage to joint. The second what was the nature of the pathology that provoked such an osteolytic lesion to cause this fracture with this simple fall in a young active male.
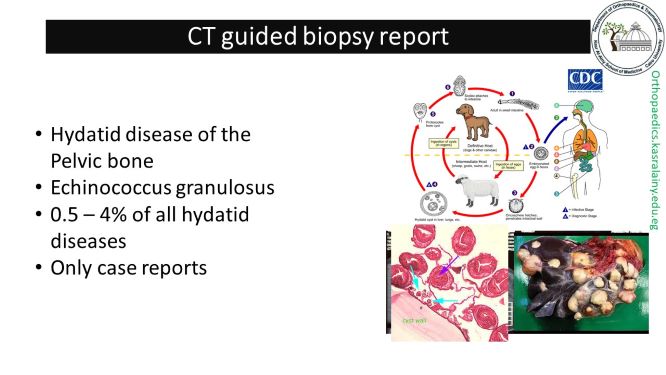
A CT guided biopsy was done for which the diagnosis for Echinococcus granulosis was confirmed. The literature reports only a few case affecting the musculoskeletal system least of all the pelvis and acetabulum
The surgical options were confusing. There was a need for surgical intervention for both resection and treatment of the lesion as well as managing the acetabular fracture. The 3 possible options would be reconstruction of the fracture meaning open reduction and internal fixation or arthroplasty with acute primary replacement.
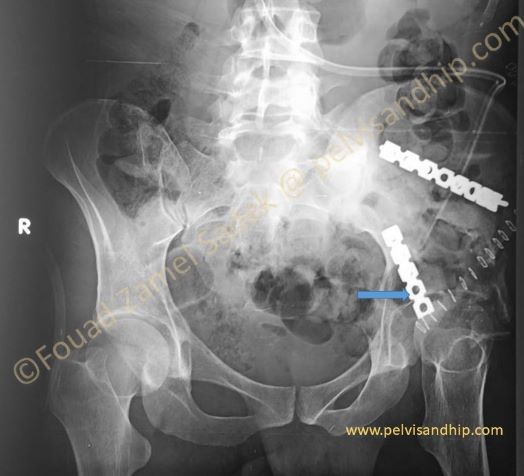
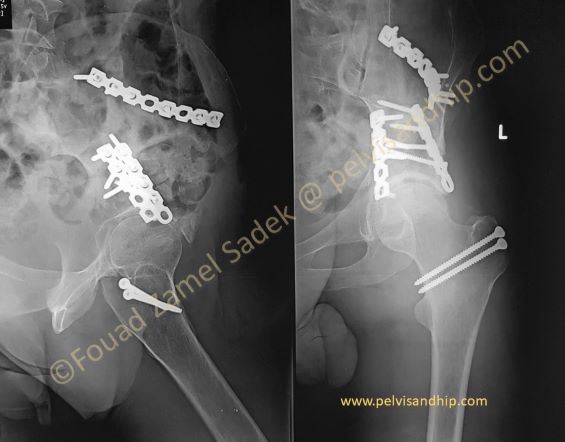
Considering our patient’s young age and our conviction of always to attempt at hip preservation; the plan was to do an acetabular reconstruction with open reduction and internal fixation. Decision was to carry out a combined approach with an anterior ilioinguinal approach first with a short segment fixation. This was approached through the lateral and middle windows primarily to gain adequate access into the cyst which needed to be carefully and meticulously curetted to avoid recurrence something we all know hydatic disease have a propensity to do. The proximal high anterior column was reduced and fixed with a second buttress plate (blue arrow) applied for the anterior wall fracture. One can see that the hip is still in external rotation with some tendency for superolateral subluxation; something that needs to be fixed with the second approach.
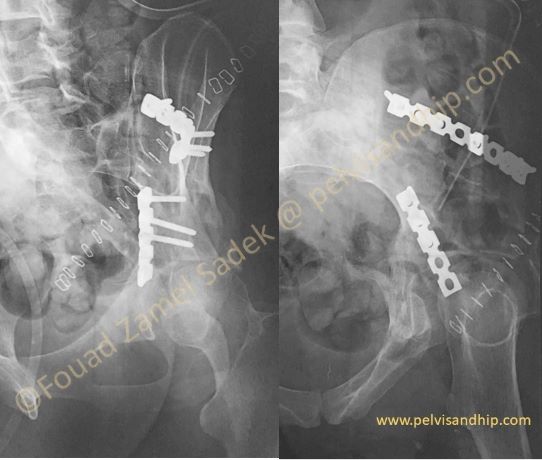
The oblique views show the result after the first stage whereby the dome fracture is well seen on the obturator oblique views.
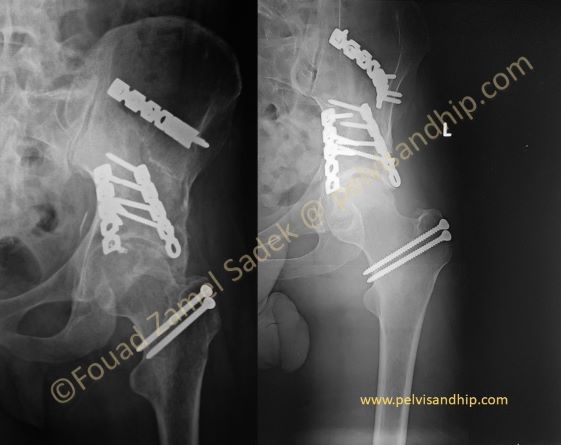
The second stage consisted of a posterior Kocker-Langenbeck approach with an added surgical dislocation with a trochanteric flip to gain perfect access into the dome of the acetabulum. The dome was well reduced and fixed with superior plating. Bone graft was taken from the intact iliac crest to be applied at the subchondral area of the cyst to support the very thin and weak cartilage.

One year follow up shows the fracture to have been completely united with bone filling of most of the cyst and no fixation failure. There are some radiological changes of early arthritic changes but clinically the patient had no pain and he was back to work in an office. His main complain was related to some block in acute flexion which is probably do to extra bone formation along the anterior and superior aspect of the joint. (blue arrow)

2 years follow up x-rays showed the preserved joint space and the lateral extension of the excessive bone formation (blue arrow) while the patient was clinically functioning fairly well with the hip with only a complain about the flexion block.
At the 3 years mark, he underwent excision of the excessive bone formation through an another approach similar to a direct anterior approach without opening the capsule. Resection was rather straight forward with excellent improvement of the range of motion.
At the 3 years mark, he underwent excision of the excessive bone formation through an another approach similar to a direct anterior approach without opening the capsule. Resection was rather straight forward with excellent improvement of the range of motion. You can see the difference before (left side) and after (right side) excision of the excess bone. After more than 3 and half years from the index surgery, there was no recurrence of the lesion and hip function is satisfactory.

Learning point: 1. careful assessment of pathological fractures of the acetabulum is mandatory to identify the case of the osteolysis can influence the choice of treatment. 2. the treatment of acetabular fractures should always be aimed at joint preservation especially for the young and active. 3. The surgical approach has to be carefully planned with the view on what needs to be done; in this case more extension of the ilioinguinal approach to the middle window (instead of just the lateral window) for better access for curettage of the bone lesion. 4. The trochanteric flip extension of the posterior approach is very useful to gain access to the intraarticular compartment. 5. Follow through with tailoring of further surgical interventions is needed to provide the patient with the best functional result.